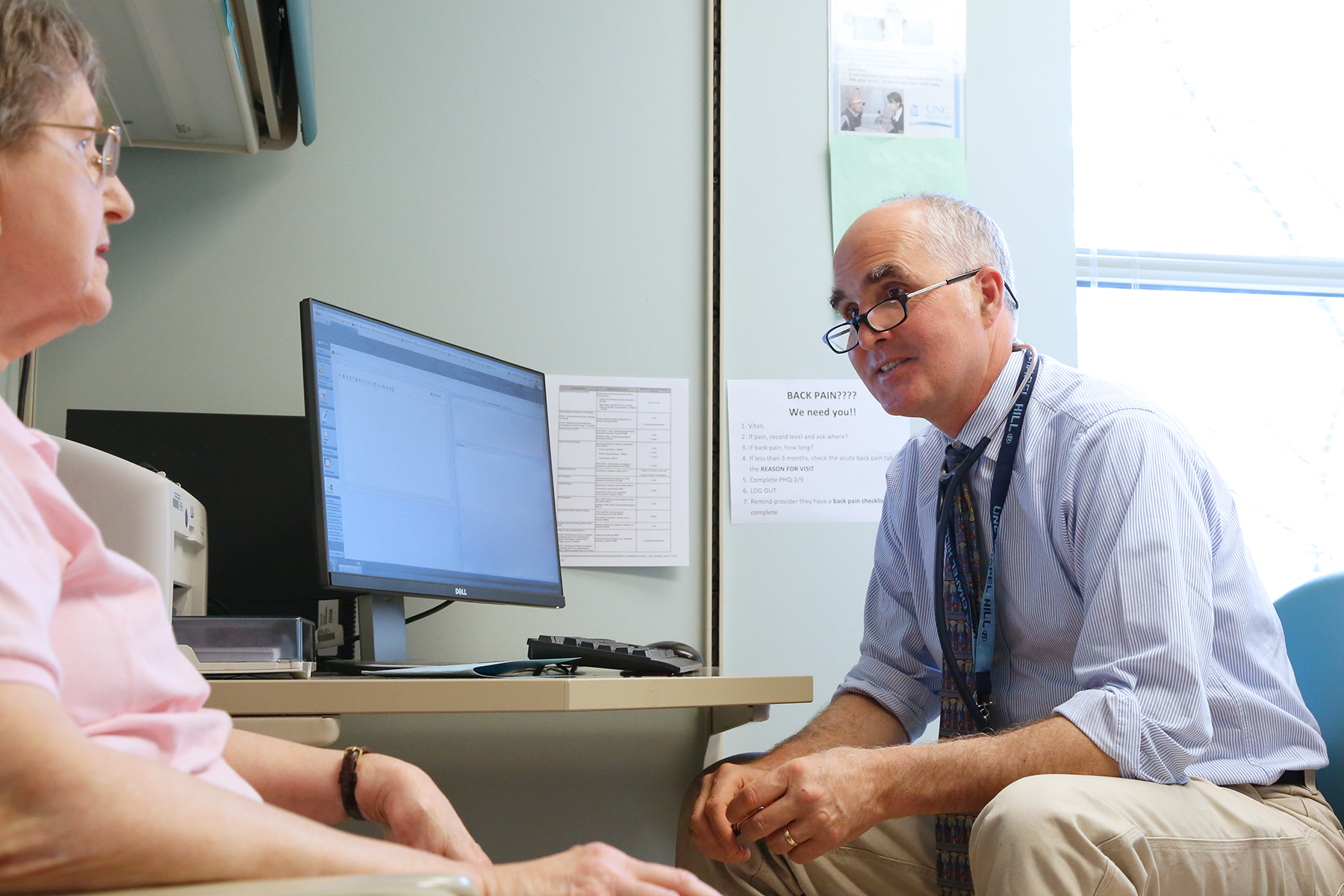
UNC’s Paul R. Chelminski, MD, MPH, and Timothy J. Ives, PharmD, MPH, CPP, have been sounding the alarm about proper opioid prescribing for decades. Now their treatment methods are the focus of a multi-institutional study on opioid use that could one day change how all health care providers approach chronic pain management.
(Excerpts republished from the UNC Health Care and School of Medicine Newsroom)
Paul Chelminski, MD, has been researching alternative methods for managing chronic pain since the early 2000s. He’s also been warning physicians about the consequences of over-prescribing opioids for just as long.
“In the 1990s when the use of opioids was first promoted for chronic pain, the recommendation was that patients be carefully selected and that opioid treatment occur with close monitoring of psychological status. Neither occurred,” said Dr. Chelminski in an article from the UNC Health Care and School of Medicine Newsroom. “No pain medication was ever intended to become the mainstay of pain treatment. Unfortunately, as patients became more dependent on opioids, providers became equally dependent on prescribing them as the centerpiece of treatment.”
Chelminski says multiple things contributed to this view of opioids and pain. The Joint Commission–a non-profit which accredits more than 21,000 U.S. health care programs and organizations–introduced its Pain Management Standards in 2001. Those standards led to pain becoming the fifth vital sign, requiring physicians to ask patients to rate the amount of pain they’re experiencing. This created concern amongst doctors that they would be judged on their patients’ discomfort, not their ultimate care. Chelminski says this atmosphere – coupled with inaccurate representation and marketing of opioids by pharmaceutical companies – led to a culture of prescribe first, ask questions later. It’s a culture he and fellow UNC physicians have been trying to break.
“In many respects, we’re an opioid reduction service,” said Timothy Ives, PharmD, professor of pharmacy at the UNC Eshelman School of Pharmacy, adjunct professor of medicine and director of the Pain Management Program in the Division of General Medicine and Clinical Epidemiology at the School of Medicine. “If the patient doesn’t have a true indication for opioids, then we start them on the targeted medications that they do need.”
Ives and Chelminski worked together on a study in 2006 that found opioid misuse occurred frequently – about one-third of the time – in chronic pain patients in a pain management program within an academic primary care practice. It was concluded that chronic pain is often accompanied by psychiatric comorbidity and disability, and they suggested that structured monitoring for opioid misuse can potentially ensure the appropriate use of opioids and reduce adverse public health effects of diversion.
Chelminski and Ives closely monitor their own patients for the depression and anxiety that often complicate chronic pain. Ives said chronic pain can sometimes be manifestations of mental health issues, rendering opioids useless as a treatment. He said in other patients severe pain can affect mood and personality. Both are reasons why he often advises his patients to see a psychologist or psychiatrist, which can ultimately aid in creating a treatment method that suits each individual patient’s needs, with or without opioids.
Cognitive behavioral therapy (CBT) is a behavioral and psychological intervention that has shown great promise in improving pain outcome and has become the intense focus of research interest among physicians who treat patients with pain. “These treatments allow patients to explore how they cope with illness and the pain,” explained Chelminski. “CBT has been shown in counseling and behavioral health settings to be very effective in helping patients with chronic pain, but it hasn’t been systematically tested as an intervention in primary care or pain clinics.”
Chelminski and Ives are part of a multi-institutional study to investigate how CBT and motivational interviewing (MI) can reduce the use of opioids for patients managing chronic pain. The $9 million study funded by the Patient-Centered Outcomes Research Institute (PCORI) is led by RTI International and also includes the Mid-South Clinical Data Research Network, which is centered at Vanderbilt University Medical Center, and includes Duke University Health System and the UNC Health Care System. UNC will recruit around 300 of the 1,000 chronic pain patients involved, mostly from UNC’s Pain Center.
“This clinical trial is intended to retrofit pain management and align it with the sensible recommendation that chronic pain therapy should incorporate a strong behavioral medicine component,” said Dr. Chelminski, a principal investigator of the study.
The study will compare two interventions to evaluate their effect on opioid dosage, physical functioning and pain-related outcomes. One intervention involves a shared decision-making process where patients and clinicians make evidence-based decisions together that align with the patients’ preferences and values. The other intervention, in addition to the shared decision-making process, uses MI as a goal-oriented counseling technique to enhance an individual’s motivation for behavior change. CBT in group sessions to foster more positive thoughts, emotions and behaviors to help manage pain.
Both Ives and Chelminski have high hopes for the outcome of the study. From their own individual practices they’ve learned what a difference integrating mental health services can make in the treatment of chronic pain. They say this is a chance to prove it on a larger scale and potentially change the way health care providers manage pain by integrating mental health services into all care, especially substance misuse disorders.
Ives said, “My hope is that we can put together a model that can be translated to numerous types of outpatient settings that really gets people more functional with less medication and less medical interventions, and at the same time maintains or improves their quality of life.”
Find the full article here.