A new schedule model for the Internal Medicine Residency Program will foster more resiliency, greater access to subspecialty mentorship and outpatient experiences, improve continuity within primary care clinics, and provide several layers of mentorship and support as residents move from trainee to fully licensed physician.
Resident schedules in the Department of Medicine have traditionally consisted of 7-8 months of inpatient service requirements and 4-5 months of outpatient clinic and consult services. One month long inpatient rotations were randomly distributed throughout the academic year, and in some cases, meant 4-5 month stretches of inpatient work without reprieve. This often resulted in resident burnout and inadequate time to schedule continuity clinics. Since the continuity with patients in the primary care clinic is a key driver for resident satisfaction, prolonged stretches of inpatient service have been shown to undermine the long-term relationship building aspect of primary care.
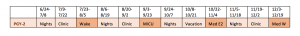
Starting this year, all current and future residents will work two weeks of inpatient days, two weeks of inpatient nights, followed by two weeks of outpatient days. This six-week cycle will repeat eight times throughout the academic year. The entire residency will be divided into three cohorts (one-on-days, one-on-nights and one-on-outpatient days at any given time), in an effort to foster natural peer-mentor groups.

Chief Resident Benjamin Sines, MD, led the effort to rethink the traditional schedule model. He says the gradual increase in the residency size over the last four years made a redesign possible, which will not only distribute demanding inpatient service requirements more equitably across the academic year while improving continuity with patients, it will give residents more opportunities to pursue subspecialty interests.
“The majority of residents who train in internal medicine will ultimately continue their training in a subspecialty field, and most of this exposure to subspecialty medicine comes during inpatient rotations,” said Sines.
“Our new schedule will allow trainees to identify mentors in their chosen subspecialty and rotate through their outpatient clinics at regularly scheduled intervals, creating a subspecialty continuity clinic. This longitudinal relationship between the mentor and trainee will also foster more productive research opportunities for residents and create peer-mentor groups for academic enrichment and coverage needs.”